Does Insurance Cover the Costs of Inpatient Teen Treatment Programs
By PAGE Editor
If you’re a parent concerned about your teen’s mental health or substance use, one of the first questions you’re likely to ask is: does insurance cover the costs of inpatient teen treatment programs?
The short answer is yes, in many cases, insurance can help pay for inpatient treatment for teens.
However, the exact coverage depends on several factors, including your specific insurance plan, the treatment center's accreditation, the medical necessity of the services, and whether the facility is in-network.
Understanding how insurance works in this context can give you the confidence and clarity you need during what is often a stressful and emotional time.
Our resource from ReveriePAGE breaks down the details you need to know in order to get essential services covered for your struggling teen.
Understanding Inpatient Teen Treatment and Why It Matters
Inpatient treatment programs for teens provide 24/7 care in a structured environment. These programs typically address mental health disorders such as anxiety, depression, trauma-related issues, behavioral disorders like oppositional defiant disorder (ODD), or substance use problems.
Unlike outpatient care, inpatient treatment offers intensive therapeutic support, medical supervision, and a safe space for teens to heal.
When a young person is in crisis, early intervention through a residential or inpatient program can prevent long-term complications and help set them on a path toward recovery and healthy development.
Many families exploring finding inpatient programs for your teen discover that choosing the right program is only part of the challenge—the other part is figuring out how to pay for it.
How Insurance Coverage for Inpatient Teen Treatment Works
So, does insurance cover the costs of inpatient teen treatment programs? Generally speaking, most health insurance plans—whether private, employer-sponsored, or government-backed—offer some level of behavioral health coverage, including inpatient psychiatric or addiction treatment for teens.
This is due in part to the Mental Health Parity and Addiction Equity Act (MHPAEA), which requires insurance providers to offer mental health and substance use treatment benefits that are comparable to medical and surgical benefits.
Additionally, the Affordable Care Act (ACA) mandates that behavioral health services be considered essential health benefits. That said, the extent of coverage varies. Plans may cover part or all of the treatment costs, depending on factors like deductibles, copays, out-of-pocket maximums, prior authorization requirements, and the provider’s in-network status.
Factors That Determine Whether Insurance Will Pay
When evaluating whether your insurance will cover inpatient teen treatment, keep the following key considerations in mind:
1. Medical Necessity – Insurance companies typically require a licensed clinician to determine that inpatient treatment is “medically necessary.” This means the child’s symptoms or behaviors must warrant a level of care that can’t be safely provided in an outpatient or lower-intensity setting. A formal psychological assessment or referral from a doctor or therapist can support this.
2. In-Network vs. Out-of-Network – Coverage levels differ depending on whether the treatment center is in-network with your insurance provider. In-network facilities have negotiated rates with insurers, which can lower your costs. Out-of-network programs may still be reimbursed partially, but they often come with higher out-of-pocket expenses.
3. Type of Plan – Your plan type—HMO, PPO, EPO, or POS—can influence coverage. HMOs usually require referrals and restrict you to a defined network, while PPOs offer more flexibility with provider choice.
4. Level of Care – Some insurance plans only cover certain levels of care. For instance, a plan may cover psychiatric inpatient hospitalization but not long-term residential treatment. Always clarify the distinction with your insurer.
5. Prior Authorization – Many insurers require pre-approval before they’ll authorize coverage for inpatient services. This means you or your provider must submit documentation showing the medical necessity of treatment before admission.
What’s Typically Covered by Insurance in Inpatient Teen Treatment?
When coverage is approved, insurance may cover a wide range of services within the inpatient teen program. These often include:
● Room and board
● Psychiatric evaluations
● Individual and group therapy
● Medication management
● Recreational therapy
● Family therapy sessions
● Case management and discharge planning
Some plans may also include aftercare or step-down services such as intensive outpatient programs (IOP) or partial hospitalization programs (PHP), depending on your child’s recovery needs.
Common Insurance Challenges Families Face
Navigating insurance for inpatient teen treatment can feel overwhelming. Here are some common challenges families report:
Denied Claims – Sometimes, insurers deny claims on the grounds that the treatment wasn’t medically necessary, the facility was out-of-network, or there was a lack of proper documentation.
Short Coverage Durations – Even when coverage is approved, it may be limited to short stays (e.g., 10–14 days), after which further authorization is required to continue care.
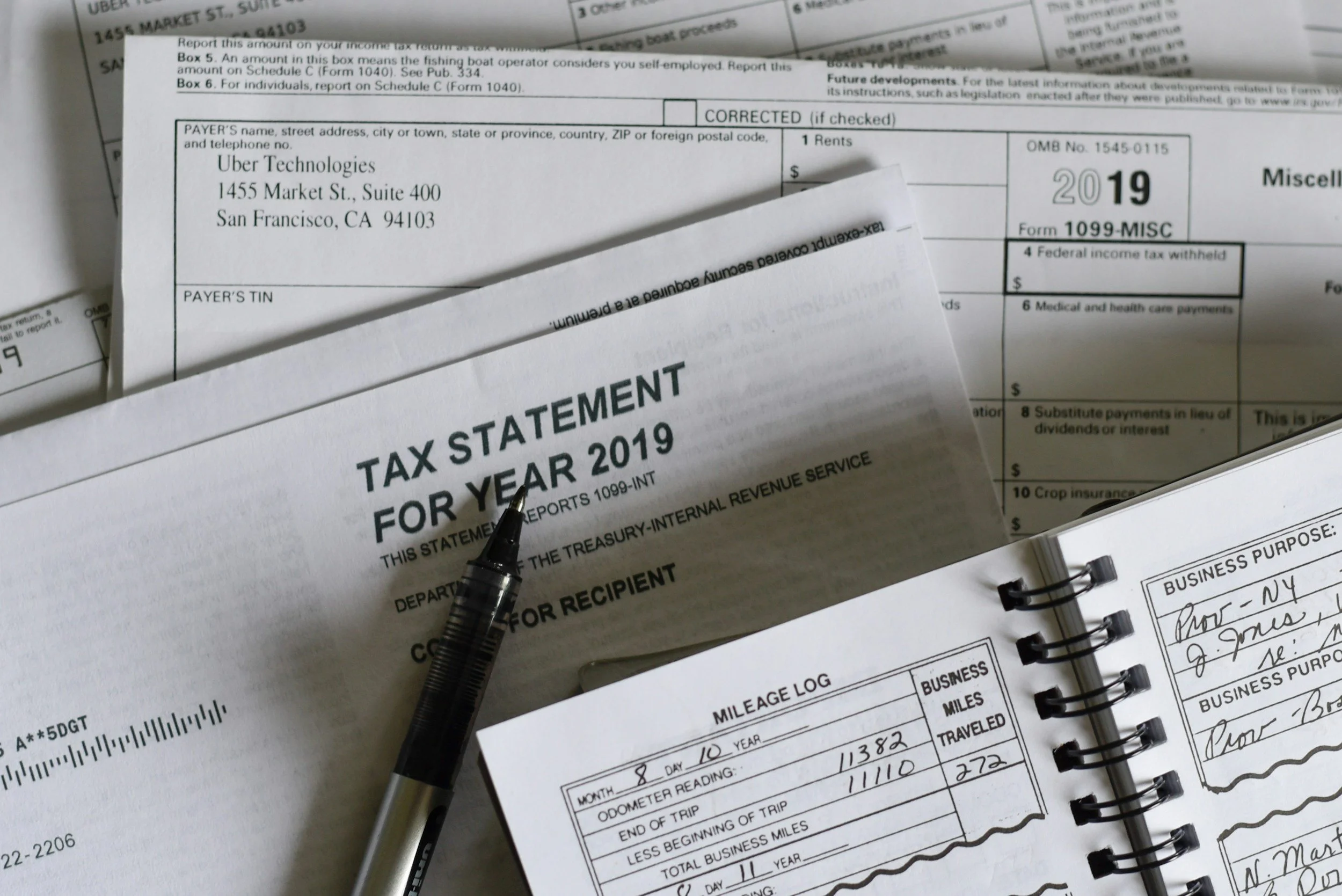
Billing Confusion – Parents often struggle to understand explanations of benefits (EOBs), itemized bills, and statements from both the provider and the insurance company.
High Out-of-Pocket Costs – Deductibles, copays, coinsurance, and balance billing can all add up, even with insurance.
5 Tips for Maximizing Your Insurance Benefits
To improve the likelihood of insurance coverage for your teen’s inpatient treatment and reduce stress, try the following tips:
1. Call Your Insurance Provider First – Ask for a detailed explanation of your behavioral health benefits. Request written confirmation if possible.
2. Request a Case Manager – Some insurance companies assign case managers to help families navigate care options and paperwork.
3. Choose an Accredited Program – Opt for a treatment center that is licensed and accredited (e.g., by the Joint Commission or CARF), as insurers are more likely to approve coverage.
4. Ask About Financial Assistance – Many reputable treatment centers offer flexible payment plans, scholarships, or sliding-scale options for out-of-pocket costs.
5. Keep Records of Everything – Maintain a file with all correspondence, assessments, billing records, authorization letters, and appeals. This can be crucial if you need to contest a denial.
Alternatives if Insurance Doesn’t Fully Cover Treatment
If your insurance only covers part of the cost—or denies coverage entirely—there are still options available. Some families consider:
● Health Savings Accounts (HSAs) or Flexible Spending Accounts (FSAs) to pay for eligible medical expenses
● Financing options through third-party lenders
● State and local behavioral health programs that offer free or reduced-cost services
● School-based referrals that can lead to therapeutic day schools or public services
● Nonprofit grants and advocacy organizations that support families in crisis
Choosing the Right Program for Your Teen
Coverage is only part of the picture—choosing the right facility is just as important. Look for programs that offer individualized treatment plans, a licensed and experienced clinical team, and a strong family involvement model.
Whether you’re seeking care close to home or are open to out-of-state options, you want a program that not only treats symptoms but also empowers your child to thrive academically, socially, and emotionally.
If you’re exploring options in the Southwest, consider that Tucson offers Artemis Adolescent Healing Center, a leading Arizona rehab for adolescents, which often blends evidence-based therapy with holistic and experiential activities in a serene environment designed for healing.
What to Expect in the Admissions Process
The admissions process for inpatient teen treatment typically includes an intake assessment, insurance verification, a clinical review to determine medical necessity, and a pre-admission call.
During this process, the admissions team will help guide you through insurance paperwork, discuss your financial responsibility, and coordinate logistics such as transportation and what to pack.
Reputable programs will work closely with you to remove as many barriers as possible to getting your teen the care they need.
Let Insurance Form a Bridge to Help, Not a Barrier
Navigating insurance coverage for inpatient teen treatment can be daunting, but it shouldn’t stand in the way of your child’s healing journey. The key is to become an informed advocate—understand your rights, work closely with the treatment center, and don’t hesitate to ask questions.
While there may be some hurdles, insurance is often a critical bridge to accessing high-quality care. Whether you’re still researching your options or are already deep into finding inpatient programs for your teen, remember that help is available, and you are not alone.
If you need more guidance or a personalized consultation, reach out to a trusted provider who specializes in adolescent behavioral health. They can help walk you through the process, from insurance verification to admission and beyond—so you can focus on what matters most: your teen’s well-being and future.
FAQs About Insurance and Teen Treatment
Will my insurance cover the entire cost of treatment? It depends. Some plans cover 100% after the deductible is met, while others may require coinsurance or copays.
Do I need a referral from a doctor? Not always, but some insurance plans—especially HMOs—do require one. It’s best to check directly with your provider.
Can I choose any facility I want? If the program is out-of-network, you may face higher costs or limited coverage. It’s wise to prioritize in-network options when possible.
What if my insurance denies coverage? You can appeal the decision. Ask the treatment center for help gathering medical records and writing appeal letters.
Will insurance cover follow-up care after inpatient treatment? Most insurance plans do cover aftercare such as outpatient therapy or IOP, but you may need new authorizations for these services.
HOW DO YOU FEEL ABOUT FASHION?
COMMENT OR TAKE OUR PAGE READER SURVEY
Featured




When investing in quartz countertops, choosing the right warranty and care package is just as important as selecting the color and finish.